
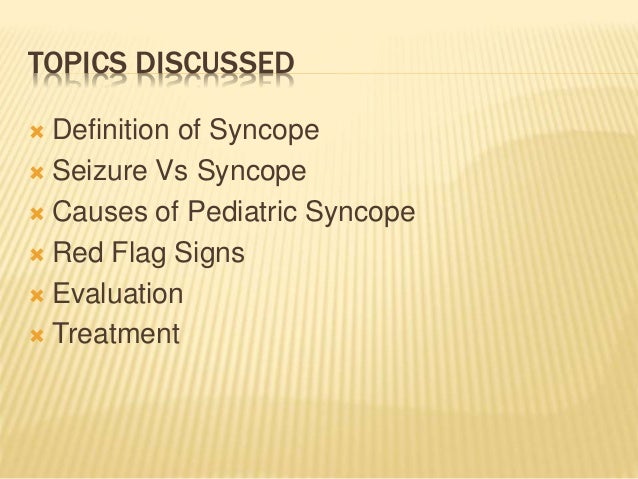
Patients with apparent syncope should be evaluated for potential immediate life-threatening conditions. History and physical examination can help guide further diagnostic evaluation and management. For patients presenting with apparent syncope, immediate treatment should focus on identifying and treating life-threatening conditions. Many laboratory studies and imaging can be nondiagnostic during ED evaluation. Other nonemergent conditions include cataplexy, pseudosyncope, or deconditioning. Some of the most emergent conditions include seizures, stroke, metabolic disorders, and head trauma. Reflex syncope is the most frequent cause of fainting. This causes blood pressure to drop, so less blood flows to the brain and fainting (syncope) or near-fainting (pre-syncope) occurs. Many conditions can present similarly to syncope, making diagnosis in the ED difficult. Reflex syncope is the result of a reflex response to some trigger, in which the heart slows or blood vessels dilate (widen). Syncope is caused by transient LOC secondary to global cerebral hypoperfusion. This review evaluates patients presenting with a history concerning for possible syncope, mimics of syncope, and approach to managing syncope mimics. The symptoms and presentation of syncope are similar to many other conditions, which can lead to difficulty in establishing a diagnosis in the ED. When this happens during waking, the patient who had a cataplectic attack loses muscular control. This loss of tonus is caused by massive inhibition of motor neurons in the spinal cord. The transient nature of the event can make diagnosis in the emergency department (ED) difficult, as symptoms have often resolved by time of initial presentation. Theories for episodes A phenomenon of REM sleep, muscular paralysis, occurs at an inappropriate time. All rights reserved.Syncope is an event that causes a transient loss of consciousness (LOC) secondary to global cerebral hypoperfusion. 6, P 0.002), whereas fewer had a diagnosis of pseudo-syncope (6 vs. 46, P 0.001) and orthostatic syncope (10 vs. TIA carotid sinuy syndrome cataplexy cough syncope drop attacks epilepsy neurally mediated syncope otrhostatic hypotension psychogenic spells seizures sleep attacks subclavian steal syndrome syncope transient loss of consciousness vasovagal attacks. More standardized-care patients had a diagnosis of neurally mediated (65 vs. Management strategies involve pharmacologic and nonpharmacologic interventions, and cardiac pacing. Cataplexy, effectively REM (rapid eye movement) sleep intruding into wakefulness.
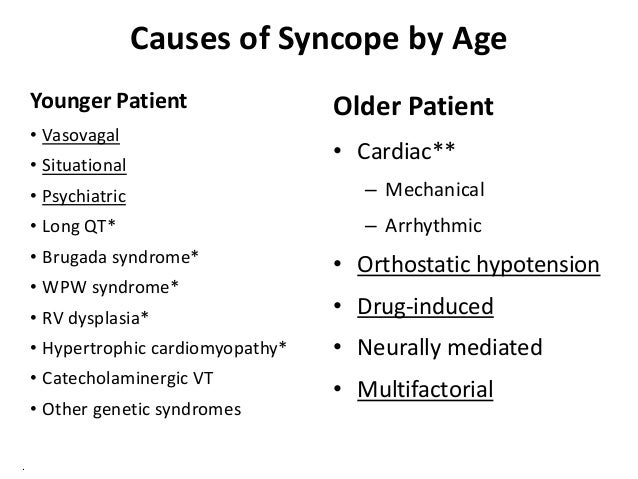
Blood testing, electroencephalogram (EEG), magnetic resonance imaging (MRI) of the brain, echocardiography, head-up tilt test, carotid sinus massage, Holter monitoring, and loop recorders should be obtained only in specific contexts. Clinical distinction of reflex (vasovagal) syncope from seizures. Basic diagnostic workup of TLOC includes a thorough history and physical examination, and a 12-lead electrocardiogram (ECG). Syncopal episodes may or may not be preceded by prodromal symptoms, which are described below. Nonsyncopal TLOC may be due to neurologic (epilepsy, sleep attacks, and other states with fluctuating vigilance), medical (hypoglycemia, drugs), psychiatric, or post-traumatic disorders. Syncope is a transient, self-limited loss of consciousness caused by transient, self-terminating, inadequate nutrient flow to the brain. Rarely neurologic disorders (such as epilepsy, transient ischemic attacks, and the subclavian steal syndrome) can lead to cerebal hypoperfusion and syncope.
The most common causes of syncopal TLOC include: (1) cardiogenic syncope (cardiac arrhythmias, structural cardiac diseases, others) (2) orthostatic hypotension (due to drugs, hypovolemia, primary or secondary autonomic failure, others) (3) neurally mediated syncope (cardioinhibitory, vasodepressor, and mixed forms). The term TLOC is used when the cause is either unrelated to cerebral hypoperfusion or is unknown. Syncope describes a sudden and brief transient loss of consciousness (TLOC) with postural failure due to cerebral global hypoperfusion.


 0 kommentar(er)
0 kommentar(er)
